Voir la vidéo
- Regardez la vidéo sur youtube

Champignons de la peau - Pityriasis Versicolor
Appelés aussi mycètes, les champignons sont couramment présents dans la flore cutanée et dans l'environnement, mais ne posent généralement pas de problème ; en effet, ils ont tendance à "coexister" avec l'organisme humain à l'état saprophyte, sans causer de dommages. Tout cela grâce à plusieurs facteurs défensifs qui protègent le corps humain de leur développement excessif.
Dans certaines conditions favorables, cependant, les champignons cutanés peuvent se transformer en agents pathogènes invasifs, se comportant comme des micro-organismes opportunistes. En pratique, ces champignons sont capables « d'exploiter » un état immunitaire affaibli de l'organisme pour augmenter leurs colonies sur la peau, au point de provoquer des maladies.
Sans surprise, les infections causées par les champignons cutanés sont plus fréquentes durant l'été, lorsque la chaleur et l'humidité typiques de la saison estivale facilitent leur croissance et leur propagation entre les individus (étant donné la fréquentation des lieux surpeuplés, comme les piscines et les plages).
Les symptômes associés à la mycose de la peau se manifestent dans les sites cutanés et dans les structures attachées (par exemple le cuir chevelu, les ongles, les organes génitaux ou la surface de la peau) qu'ils infectent.
L'épidémiologie varie d'une forme de mycose à l'autre et est largement influencée par de multiples facteurs environnementaux et subjectifs.
Le diagnostic repose sur l'aspect clinique des lésions, détectées à l'examen dermatologique, et sur l'examen microscopique et culturel du tissu infecté.
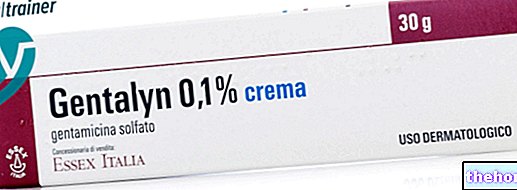
Le traitement dépend du site de l'infection, mais implique généralement l'utilisation d'antifongiques topiques ou oraux, visant spécifiquement le champignon cutané en question.
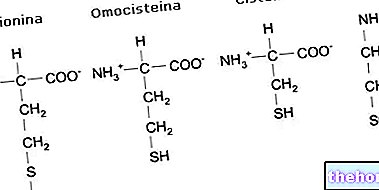
de plantes ou d'animaux. Les experts en mycologie sont capables d'identifier et de classer les champignons en fonction de leur apparence microscopique et de leur mode de reproduction, qui peut se produire à la fois sexuellement et asexuée. Les champignons qui infectent la peau humaine sont de taille microscopique et peuvent être unicellulaires de forme ovoïde (comme les levures) ou multicellulaires et filamenteux (comme les moisissures).Les espèces appartiennent à cette catégorie Epidermophyton, Microsporum Et Trichophyton.
Les dermatophytes sont responsables de macules cutanées caractéristiques en forme de rosette, à arêtes vives et à évolution centrifuge (teigne). Certains de ces champignons peuvent infecter le tronc (tinea corporis), les pieds (tinea pedis ou pied d'athlète), les ongles (tinea unguium) et les plis inguinaux (tinea cruris).Ces infections représentent environ 40 à 50 % de toutes les mycoses superficielles et diffèrent des candidoses en ce qu'elles ne sont que rarement invasives.

Champignons de la peau - Pied d'athlète (Pied d'athlète)
- Levures : ce sont des micro-organismes unicellulaires et non filamenteux qui se reproduisent très rapidement de manière asexuée, se localisant dans les zones chaudes-humides du corps (cavité buccale, aisselles, plis sous-mammaires, espaces interdigitaux, région anogénitale…).
De nombreuses levures sont normalement présentes sur la peau et ne causent pas de dommages (elles coexistent presque toujours à l'état saprophyte).
Les levures les plus importantes en dermatologie sont : Candida albicans, Malassezia furfur Et Cryptococcus neoformans.
Selon l'agent fongique responsable et la zone du corps touchée, les manifestations cutanées visibles peuvent inclure un œdème, des rougeurs et des plaques desquamatives blanc rosé ; des démangeaisons sont presque toujours présentes. - Moisissures : sont des champignons multicellulaires et filamenteux qui se reproduisent sexuellement.
Les moisissures pathogènes les plus courantes sont : Alternaria, Aspergillus Et Fusarium. Ces types de champignons sont principalement responsables de mycoses profondes et systémiques, alors que ce n'est que dans de rares cas qu'ils provoquent des infections cutanées et superficielles.
En général, ces pathologies peuvent être divisées en deux types :
- Superficiel et cutané : limité à la couche superficielle de la peau (épiderme), des cheveux, des ongles et des muqueuses (cavité buccale et génitaux) ;
- Sous-cutanée : étendue au derme et aux structures connectées.
Les maladies de la peau dues aux champignons peuvent affecter tout le monde, indépendamment du sexe et de l'âge. Dans la plupart des cas, les personnes qui développent des mycoses cutanées ont une réponse immunitaire réduite, par exemple en raison d'une « altération des défenses locales (ex : traumatisme avec atteinte vasculaire) ou » d'une immunosuppression (ex : diabète, SIDA, dysbiose antibiotique, etc.).
La transmission peut se produire de personne à personne, d'animal (chat, chien, lapin, souris et bétail) à personne et, rarement, de sol et d'objets contaminés à l'homme.
Les mycoses cutanées les plus fréquentes sont :
- Dermatophytose : Infections fongiques touchant les zones kératinisées du corps (stratum corneum, cheveux ou ongles). Les symptômes peuvent varier, mais il s'agit la plupart du temps de lésions cutanées, qui démangent rarement.
- Candidose : mycoses qui affectent principalement les zones de sudation, telles que l'aine, les aisselles et les zones interdigitées. Au niveau des muqueuses, de la cavité buccale (ex. muguet), des organes génitaux (ex. vulvovaginite de Candida albicans) et l'œsophage (en particulier chez les sujets immunodéprimés).
- Pityriasis versicolor : infection fongique de la peau dans laquelle de petites taches plates et inégales apparaissent sur le cou, le tronc, l'abdomen, les bras et le visage.
La caractéristique de la maladie est l'altération de la pigmentation de la peau (dyschromie) : les lésions sont hypo ou hyper pigmentées et prennent une couleur allant du blanc au brun.Les zones cutanées colonisées, en effet, si elles sont exposées au soleil, gênent la passage des rayons ultraviolets qui, dans des conditions normales, stimulent la production de mélanine.
Ces conditions comprennent :
- Mauvaises habitudes alimentaires;
- Hygiène insuffisante;
- Stress physique;
- Humidité chaude et excessive;
- Situations de macération cutanée chronique (transpiration excessive, habitude de porter des vêtements peu respirants) ;
- Traitements prolongés à base d'antibiotiques ou de cortisone ;
- Défense immunitaire compromise par des pathologies particulières (SIDA, tumeurs, diabète, etc.) ;
- Prendre des médicaments immunosuppresseurs.
Dans certaines infections fongiques, les lésions sont d'abord blanchâtres, puis ont tendance à s'assombrir avec le temps.
La plupart du temps, l'inflammation est faible ou inexistante, mais parfois, lorsque l'inflammation est plus sévère, elle implique des dommages aux structures impliquées, se manifestant par une soudaine formation de cloques ou une maladie bulleuse (généralement au niveau des pieds) ou par une "grande Lésion molle du cuir chevelu qui se traduit par des zones d'alopécie (kérion).
D'autres symptômes associés aux champignons cutanés comprennent une sensation de brûlure, des cloques et des fissures d'apparition soudaine (en particulier dans les pieds), un épaississement des ongles et une desquamation du cuir chevelu ressemblant à des pellicules.
Pour le diagnostic différentiel, le médecin peut également utiliser la lampe de Wood, qui est capable de détecter une fluorescence typique (par exemple le jaune doré de la Malassezia, verdâtre pour les dermatophytes, etc.) et excluent ces dermatoses infections non causées par des champignons.
Une fois le type de champignon cutané responsable des symptômes cliniques identifié (par culture), le médecin peut prescrire un traitement spécifique.
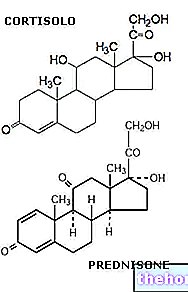
topiques (comme l'hydrocortisone) Les corticostéroïdes oraux sont rarement utilisés pour traiter les lésions inflammatoires sévères.
Pour en savoir plus : Médicaments pour le traitement des mycoses cutanées », modifient le pH de la peau et favorisent la stagnation de l'humidité.