La bonne nouvelle est que de nombreuses tumeurs ne sont pas très agressives, restent confinées à la prostate et ont une évolution plutôt lente ; cela signifie que les patients peuvent vivre avec un cancer pendant des années sans subir de traitements spécifiques et sans subir de conséquences négatives pour leur santé. De plus, lorsque cela est nécessaire, les options thérapeutiques sont multiples et assez efficaces. Malheureusement, à côté des formes à croissance très lente, il existe également des cancers de la prostate plus agressifs, avec une tendance à la métastase. Ces types de cancer se développent rapidement et peuvent se propager à d'autres parties du corps (par le sang ou le système lymphatique), où les cellules cancéreuses peuvent former des tumeurs secondaires (métastases). Dans de telles circonstances, les chances de guérir la maladie sont très faibles.

Données en main, on estime que chaque Italien de plus de 65 ans a environ 3% de chances de mourir d'un cancer de la prostate. Pour cette raison, il est bon de ne pas baisser la garde : intervenir à temps signifie plus de chances d'éradiquer ou de contenir la maladie.
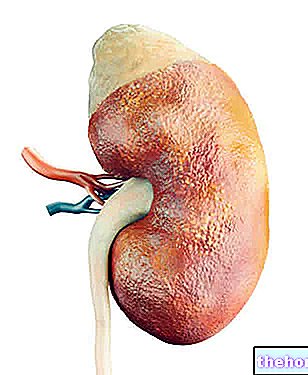
(bas de l'abdomen), juste en dessous de la vessie et devant le rectum, entourant la première partie de l'urètre. Le parenchyme est constitué d'un amas de glandes tubulo-alvéolaires, entouré d'une couche assez épaisse de fibres musculaires lisses.

La fonction principale de la prostate est d'aider à produire des spermatozoïdes, car elle sécrète une partie du liquide séminal libéré lors de l'éjaculation (remarque : le liquide séminal avec le sperme constitue le sperme).
Symptômes Cancer de la prostateAux stades précoces, le cancer de la prostate est souvent asymptomatique; cela signifie que le patient ne présente aucun symptôme, restant inconscient de la condition. Ces dernières années, grâce à la prise de conscience croissante des dangers de la maladie, la plupart des cancers de la prostate sont diagnostiqués à ces stades précoces. Un examen urologique accompagné du contrôle du PSA (antigène prostatique spécifique), au moyen de tests sanguins, permet d'identifier les sujets à risque sur lesquels effectuer des tests complémentaires.
Si la tumeur est ignorée, l'augmentation de sa taille est associée à des problèmes liés à la miction, car l'organe entoure l'urètre prostatique.Les modifications au sein de la glande affectent donc directement la fonction urinaire. Les symptômes du cancer de la prostate peuvent inclure :
- Difficulté à uriner (hésitation);
- Besoin fréquent d'uriner, surtout la nuit (nycturie);
- Difficulté à maintenir un flux régulier d'urine (le flux est faible, intermittent, ou une sensation de ne pas pouvoir vider complètement votre vessie)
- Douleur ou brûlure en urinant
- Sang dans l'urine ou le sperme
- Dysfonction érectile (impuissance);
- Éjaculation douloureuse ;
- Inconfort dans la région pelvienne;
- Fatigue, perte d'appétit et malaise général
- Douleur généralisée au dos, aux hanches ou au bassin.
ATTENTION : Les symptômes urinaires décrits se manifestent de manière similaire à d'autres troubles bénins de la prostate, comme l'hyperplasie prostatique (HBP).Pour cette raison, si une ou plusieurs de ces manifestations surviennent, il est conseillé de se soumettre à des examens médicaux spécifiques sans panique. , il pourrait en fait s'agir d'une "simple" hypertrophie bénigne de la prostate. Là encore, l'apparition de ces symptômes sous une forme aiguë pourrait indiquer une "inflammation de la prostate, généralement bactérienne : la prostatite".
Le cancer de la prostate malin peut métastaser aux ganglions lymphatiques du bassin et se propager progressivement à d'autres parties du corps. Le cancer de la prostate a tendance à se métastaser principalement aux os de la colonne vertébrale, du bassin, des côtes et du fémur. La douleur osseuse peut donc être un symptôme d'un cancer avancé de la prostate. Si la métastase comprime la moelle épinière, elle peut provoquer une faiblesse ou un engourdissement des membres inférieurs, une incontinence urinaire et fécale.
Problèmes bénins de la prostate
Les pathologies bénignes de la prostate sont plus fréquentes que les néoplasmes, surtout après 50 ans ; souvent, ces conditions provoquent des symptômes qui pourraient être confondus avec ceux de la tumeur.
Dans des conditions normales, la prostate a approximativement la taille d'une noix, mais en raison de l'âge ou de certaines pathologies, elle peut grossir et causer des problèmes, notamment urinaires.
Hypertrophie de la prostate (hyperplasie bénigne de la prostate). La prostate est très sensible à l'action des hormones, comme la testostérone.Au fil des années, un grossissement de la glande se produit spontanément, suite aux changements hormonaux qui se produisent dans le testicule (la production d'androgènes diminue et la libération de petites quantités d'œstrogènes L'hyperplasie bénigne de la prostate peut comprimer l'urètre et causer des problèmes d'urine.
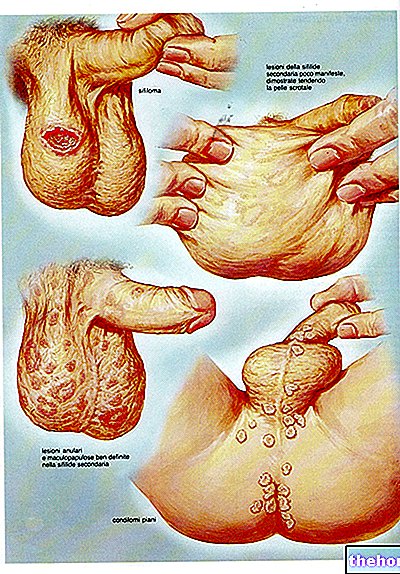
Inflammation (prostatite). La prostatite est une "inflammation de la prostate. Habituellement, la cause principale est une" infection bactérienne, mais elle peut également survenir en l'absence d'agents pathogènes. Les symptômes consistent en une douleur dans le bas-ventre, souvent accompagnée d'une dysurie, et d'une perte de sécrétions muqueuses.
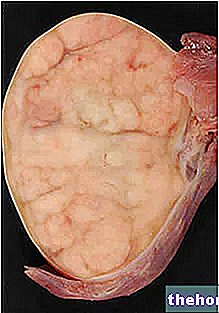
elles se caractérisent par de petites altérations de forme et de taille, qui les rendent anormales. De nombreux hommes peuvent avoir une dysplasie légère (PIN1, bas grade) même à un jeune âge, mais ils ne développeront pas nécessairement un cancer de la prostate. En revanche, une tumeur prostatique intraépithéliale de haut grade est corrélée à un risque significativement plus élevé. Pour cette raison, les médecins doivent surveiller attentivement chaque patient chez lequel il se trouve et éventuellement effectuer une autre « biopsie de la prostate ».Un adénocarcinome survient lorsque les cellules normales, constituant l'une des glandes sécrétoires, deviennent cancéreuses. Aux stades initiaux, les lésions restent confinées. Au fil du temps, les cellules cancéreuses commencent à se multiplier et à se propager dans les tissus environnants (stroma), formant une masse tumorale. Cela provoque un gonflement de la surface de la prostate, qui peut être observé lors de la palpation de la glande à travers la paroi rectale. Dans les stades ultérieurs, la tumeur peut augmenter de taille et envahir les organes voisins, tels que les vésicules séminales ou le rectum. Les cellules cancéreuses peuvent développer la capacité de migrer du site d'origine vers une autre partie du corps, par la circulation sanguine et le système lymphatique. Celles-ci peuvent proliférer et former des tumeurs secondaires. Le cancer de la prostate métastase plus fréquemment dans les os, les ganglions lymphatiques et peut envahir le rectum, la vessie et les uretères au moyen d'un mécanisme de diffusion locale.
Tumeurs malignes (cancer de la prostate)
- Ils n'envahissent pas les tissus voisins ;
- Ils ne métastasent pas dans d'autres parties du corps;
- Ils peuvent être traités et n'ont généralement pas tendance à revenir.
- Ils peuvent envahir les organes et tissus voisins (tels que la vessie ou le rectum);
- Ils peuvent donner lieu à des métastases dans d'autres parties de l'organisme ;
- Ils peuvent être soignés, mais ils peuvent revenir.
L'adénocarcinome est l'histotype le plus fréquent parmi les tumeurs prostatiques (il représente environ 95% des tumeurs malignes).
Cependant, il existe d'autres cancers, qui diffèrent par leur présentation clinique et leur évolution, notamment :
- Carcinome à petites cellules (provenant de cellules neuroendocrines);
- Adénocarcinome canalaire (provenant des cellules des canaux prostatiques);
- Carcinome mucineux (caractérisé par la production de mucus);
- Carcinome adénosquameux ou épidermoïde ;
- Tumeurs mésenchymateuses (telles que les sarcomes ou les liposarcomes);
- Lymphome primitif de la prostate.
Une fois le type de cancer diagnostiqué, le médecin devra également considérer :
- Le grade de la tumeur (comment se comportent les cellules cancéreuses anormales) ;
- Le stade du cancer, y compris s'il s'est propagé (métastasé) et où il s'est propagé
- Facteurs pronostiques (caractéristiques particulières pouvant influencer l'évolution de la maladie) ;
- Statistiques de survie pour le type particulier et le stade du cancer.
Vidéos sur le cancer de la prostate - Causes, symptômes, remèdes
Des problèmes avec la lecture de la vidéo ? Rechargez la vidéo de youtube.
- Aller à la page vidéo
- Aller à Destination Bien-être
- Regardez la vidéo sur youtube