Peu de sodium dans le sang
L'hyponatrémie représente une condition clinique dans laquelle la concentration de sodium dans le sang est inférieure à la normale.Dans les conditions physiologiques, la concentration de sodium dans le sang (natriémie ou sodémie) est maintenue à des niveaux compris entre 135 et 145 mmol/L. Oui parle de hyponatrémie (ou hyponatrémie) lorsque cette valeur tombe en dessous de 135 mmol/L.
Dans l'article précédent concernant l'hyponatrémie, nous avons attiré l'attention sur les causes déclenchantes possibles. Dans cette discussion finale, nous analyserons les symptômes qui distinguent l'hyponatrémie, les options diagnostiques et les traitements actuellement disponibles.
Symptômes
Dans l'hyponatrémie, les concentrations sériques de sodium sont réduites, il y a donc un déplacement osmotique de l'eau DU compartiment extracellulaire vers le compartiment intracellulaire.La conséquence immédiate de cet événement est un gonflement cytoplasmique.
Les statistiques médicales montrent que pour des taux de sodium supérieurs à 125 mmol/L et inférieurs à 135 mmol/L (hyponatrémie légère), les symptômes sont légers, vagues ou totalement absents. Lorsqu'il est présent, le patient affecté se plaint de symptômes gastro-intestinaux, en particulier de nausées et de vomissements. À des concentrations plus faibles en sodium, les symptômes sont accentués. Dans de telles situations, les symptômes suivants sont souvent documentés :
- Hallucinations
- Ascite (forme sévère)
- Ataxie
- Convulsions
- Crampes musculaires
- Faiblesse musculaire
- Désorientation
- Épilepsie
- Hypotension
- Mal de tête
- Perte de conscience
- Perte de mémoire temporaire
- Ralentissement des réflexes
- Bouche sèche
- Soif intense
- Somnolence sévère
- Tachycardie
Dans les cas graves, l'hyponatrémie peut entraîner un coma, une dépression respiratoire et la mort.
Plus en détail : que se passe-t-il quelques heures après le début de l'hyponatrémie ?
L'organisme réagit par une réponse adaptative : l'élimination des électrolytes des cellules cérébrales est favorisée. Un mécanisme similaire est important pour limiter autant que possible l'entrée d'eau dans le site intracellulaire.
En l'absence de traitement, au bout de quelques jours il y a une perte cellulaire de molécules osmotiquement actif (myoinositol, glycérophosphorylcholine, phosphocréatine/créatine, glutamate, glutamine et taurine).
Le risque de complications neurologiques permanentes est d'autant plus élevé que PLUS RAPIDE est la perte de ces molécules :
- Hyponatrémie chronique → les taux de sodium diminuent progressivement en quelques jours/semaines → signes et symptômes plus modérés
- Hyponatrénie aiguë → chute brutale du taux de sodium dans le sang : effets potentiellement mortels dangereux (gonflement cérébral, coma, décès)
L'hyponatrémie doit être considérée comme un phénomène pathologique grave, affectant notamment le SNC : l'œdème cellulaire peut exercer une compression sur le parenchyme cérébral, conduisant au coma et à la mort.
Diagnostic
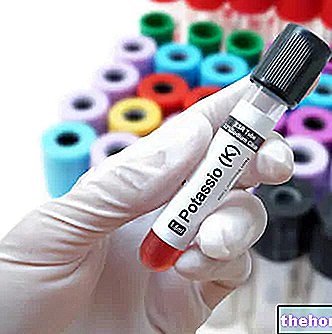
De simples antécédents médicaux et un examen physique ne suffisent pas à établir une suspicion d'hyponatrémie.Pour la confirmation du diagnostic, des analyses de sang et d'urine doivent être effectuées.
L'évaluation de la sodémie est certainement l'un des tests les plus utilisés de tous les temps : l'hyponatrémie est confirmée lorsque le taux de sodium dans le sang descend en dessous de 135 mmol/L.
La détection de sodium dans les urines > 20 mmol/L indique une hyponatrémie due à une décompensation/pathologie rénale et/ou aux hormones qui régulent son activité.
Après avoir constaté l'altération de la sodémie, il est nécessaire de procéder à un diagnostic différentiel d'hyponatrémie pour en retracer la cause déclenchante.
Dans certaines situations cliniques, des examens d'imagerie peuvent être utiles : dans le cadre d'une insuffisance cardiaque congestive, une radiographie pulmonaire est particulièrement adaptée pour constater une hyponatrémie. Une TDM cérébrale peut également être nécessaire chez les patients présentant une altération évidente de la conscience.
Thérapies
En plus d'être mal tolérées par le patient, les thérapies des formes aiguës et chroniques d'hyponatrémie sont souvent inefficaces.
Le choix du traitement de l'hyponatrémie est dicté par la cause sous-jacente et la gravité de l'affection.
L'hyponatrémie chronique légère ou modérée, causée par l'abus de diurétiques ou par une administration exagérée d'eau, doit être traitée en corrigeant la posologie des médicaments et en limitant la consommation de liquides → RESTRICTION D'EAU
Des discours différents doivent être abordés pour les formes sévères et aiguës d'hyponatrémie :
- Administration intraveineuse d'une solution à base de sodium (solutions salines hypertoniques)
- Hormonothérapie : indiquée pour les formes d'hyponatrémie dépendantes de la maladie d'Addison (insuffisance de la glande surrénale)
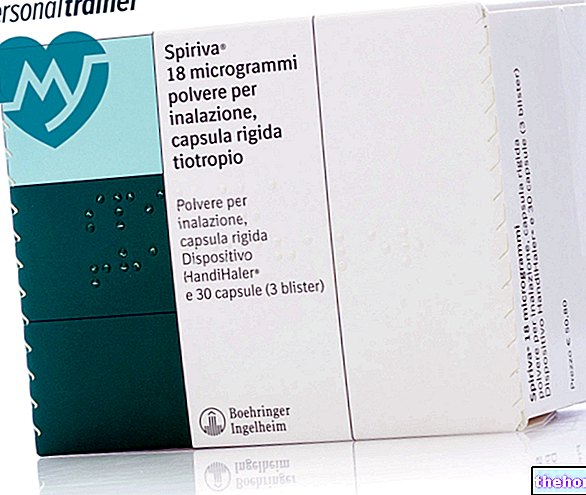
- Administration d'antagonistes des récepteurs de la vasopressine (réservé aux patients présentant une hyponatrémie associée à une cirrhose du foie, une insuffisance cardiaque congestive et un SIADH). Le tolvaptan (ex. Samsca) semble être particulièrement efficace : débuter le traitement avec une dose médicamenteuse de 15 mg, à prendre une fois par jour. La dose peut être augmentée jusqu'à 60 mg/jour afin d'atteindre un taux de sodium et un volume sanguin adéquats.
- Administration de déméclocycline ou de lithium : indiquée dans le cadre d'une hyponatrémie associée au SIADH. Ces médicaments réduisent la réactivité du tube collecteur à l'ADH.