Ingrédients actifs : Acénocoumarol
SINTROM 1 mg comprimés
SINTROM 4 mg comprimés
Indications Pourquoi Sintrom est-il utilisé ? Pourquoi est-ce?
Sintrom est un médicament appartenant au groupe pharmacothérapeutique des antithrombotiques - antagonistes de la vitamine K.
Sintrom est indiqué pour le traitement et la prévention des maladies thromboemboliques.
Contre-indications Quand Sintrom ne doit pas être utilisé
- Hypersensibilité à la substance active, aux dérivés de la coumarine apparentés ou à l'un des excipients ;
- Grossesse
- Chez les femmes en âge de procréer n'utilisant pas de mesures contraceptives (voir rubrique 4.6 "Fertilité, grossesse et allaitement").
- Patients non coopératifs et non supervisés avec un risque associé élevé de non-adhésion au traitement
Sintrom est également contre-indiqué dans tous les états pathologiques dans lesquels le risque de saignement est supérieur au bénéfice clinique possible, par exemple :
- diathèse hémorragique et/ou dyscrasie sanguine ;
- immédiatement avant ou après une chirurgie du système nerveux central, ainsi que des opérations ophtalmiques et des chirurgies traumatisantes avec exposition étendue des tissus ;
- ulcère gastroduodénal ou en présence d'hémorragie du tractus gastro-intestinal, du tractus urogénital ou du système respiratoire, ainsi qu'en cas d'hémorragies cérébrovasculaires, de péricardite aiguë et d'épanchement péricardique, et d'endocardite bactérienne ;
- hypertension sévère;
- insuffisance hépatique sévère (voir « Dose, mode et heure d'administration »);
- insuffisance rénale sévère (voir « Dose, mode et heure d'administration »);
- augmentation de l'activité fibrinolytique comme après des opérations sur les poumons, la prostate, l'utérus, etc. et dans la pancréatite aiguë;
- insuffisance circulatoire sévère avec foie de stase.
Les préparations d'Hypericum perforatum ne doivent pas être prises en même temps que des médicaments contenant de l'acénocoumarol, en raison du risque de diminution des concentrations plasmatiques et de l'efficacité thérapeutique de l'acénocoumarol (voir « Interactions »).
Précautions d'emploi Quelles sont les informations à connaître avant de prendre Sintrom
L'administration de Sintrom pendant l'allaitement nécessite des précautions (voir "Fertilité, grossesse et allaitement").
Insuffisance hépatique
Chez les patients présentant une insuffisance hépatique légère à modérée, des précautions doivent être prises car la synthèse des facteurs de coagulation peut également être altérée ou il peut y avoir un dysfonctionnement plaquettaire sous-jacent (voir également « Dose, mode et heure d'administration »). L'utilisation chez les patients présentant une insuffisance hépatique sévère est contre-indiquée (voir « Contre-indications »).
Insuffisance rénale
En raison de la possibilité d'accumulation de métabolites en cas d'insuffisance rénale, des précautions doivent être prises chez les patients présentant une insuffisance rénale légère à modérée (voir également « Dose, mode et heure d'administration »). L'utilisation chez les patients présentant une insuffisance rénale sévère est contre-indiquée (voir « Contre-indications »).
Insuffisance cardiaque
En cas d'insuffisance cardiaque sévère, un schéma posologique réduit et des contrôles de laboratoire fréquents doivent être adoptés, car l'activation ou la gamma-carboxylation des facteurs de coagulation peut être réduite en cas de congestion hépatique (voir également « Dose, méthode et heure de l'étape de récompense, cependant, il peut être nécessaire d'augmenter le dosage.
Les maladies du sang
Des précautions particulières doivent être prises chez les patients présentant un déficit connu ou suspecté en protéine C ou en protéine S car l'administration d'acénocoumarol a été associée à une nécrose tissulaire (voir « Effets indésirables »).
Population pédiatrique
Aucune étude adéquate et bien contrôlée n'a été menée dans la population pédiatrique et la dose optimale, la sécurité et l'efficacité dans cette population ne sont pas connues.
Utilisation chez les personnes âgées
Chez les patients âgés (≥ 65 ans), une attention particulière et une surveillance plus fréquente du temps de Quick et de l'INR sont recommandées (voir également « Dose, mode et heure d'administration »).
Une surveillance médicale étroite est requise dans les cas où des conditions ou des maladies peuvent réduire la liaison aux protéines de Sintrom ; par exemple, la thyrotoxicose, les tumeurs, les maladies rénales, les infections et l'inflammation.
Les troubles de l'absorption gastro-intestinale peuvent altérer l'effet anticoagulant de Sintrom.
Lors d'un traitement par anticoagulants, les injections intramusculaires peuvent provoquer des hématomes et sont donc contre-indiquées. En revanche, les injections intraveineuses et sous-cutanées n'entraînent pas de telles complications.
Traitement continu des opérations diagnostiques, dentaires et chirurgicales
Certaines procédures diagnostiques dentaires ou chirurgicales (angiographie, ponction lombaire) peuvent nécessiter une « interruption ou une modification de la dose du traitement par SINTROM. Les risques et les avantages de l'arrêt du traitement par SINTROM, même pour de courtes périodes, doivent être pris en compte. L" INR doit être déterminé immédiatement avant chaque procédure. Chez les patients subissant des procédures mini-invasives qui doivent être anticoagulés avant, pendant ou immédiatement après de telles procédures, un ajustement de la dose de SINTROM afin de maintenir l'INR au niveau le plus bas de la plage thérapeutique peut permettre en toute sécurité de maintenir le maintien. » anticoagulant.
Pendant le traitement par Sintrom, il est recommandé aux patients de porter une carte qui, en cas d'accident, avertit du traitement anticoagulant en cours.
Pharmacogénétique
La variabilité génétique notamment en relation avec les gènes codant pour les protéines CYP2C9 et VKORC1 peut influencer significativement la dose d'acénocoumarol nécessaire pour obtenir l'effet clinique recherché.Si une association avec ces polymorphismes est connue, une extrême prudence doit être exercée (voir également paragraphe 5.2).
Interactions Quels médicaments ou aliments peuvent modifier l'effet de Sintrom
Informez votre médecin ou votre pharmacien si vous avez récemment pris d'autres médicaments, même ceux sans ordonnance.
Il existe de nombreuses interactions possibles entre les coumarines et d'autres médicaments. Les mécanismes impliqués dans de telles interactions comprennent : des perturbations de l'absorption, de l'inhibition ou de l'induction du système de métabolisme enzymatique et une disponibilité réduite de la vitamine K requise pour la gamma-carboxylation des facteurs du complexe prothrombique. Il est important de noter que certains médicaments peuvent interagir avec plus de un mécanisme. Chaque thérapie peut comporter un risque d'interactions bien que toutes les interactions ne soient pas significatives. D'où la nécessité d'une surveillance attentive et de tests de coagulation fréquents (généralement deux fois par semaine) lors de la première utilisation d'un médicament en association avec Sintrom ou en cas de traitement concomitant médicament est arrêté.
Interactions pour lesquelles l'utilisation concomitante n'est pas recommandée
Effets d'autres médicaments sur l'acénocoumarol
Les médicaments suivants potentialisent l'effet anticoagulant de l'acénocoumarol et/ou altèrent l'hémostase et augmentent ainsi le risque hémorragique :
- Anticoagulants (concernant l'utilisation de l'héparine dans les situations nécessitant une anticoagulation rapide, voir « Dose, mode et heure d'administration »
- Agents antiplaquettaires
- Thrombolytiques
- Anti-inflammatoires non stéroïdiens (AINS)
- Inhibiteurs de la recapture de la sérotonine
L'utilisation de Sintrom associé à ces substances est donc déconseillée.En cas d'utilisation en association avec ces médicaments, des tests de coagulation doivent être réalisés plus fréquemment.
Interactions à considérer
Les médicaments suivants peuvent potentialiser l'effet anticoagulant de l'acénocoumarol :
Allopurinol, stéroïdes anabolisants, androgènes, agents antiarythmiques (tels que amiodarone, quinidine, propafénone), antibactériens (tels que clindamycine, pénicillines, céphalosporines de deuxième et troisième génération, chloramphénicol, macrolides, fluoroquinolones, néomycine, acide tétracyclinique), , glucagon, dérivés de l'imidazole (ex. métronidazole et, même administré localement, miconazole), paracétamol, statines, sulfamides, y compris cotrimoxazole (= sulfaméthoxazole + triméthoprime), sulfonylurées (telles que tolbutamide et chlorpropamide), hormones , tamoxifène, tramadol, pompe à protons inhibiteurs, agents procinétiques (cisapride, antiacides (hydroxyde de magnésium) et viloxazine, 5-fluorouracile et analogues, vitamine E, corticostéroïdes (tels que dexaméthasone, méthylprednisolone, prednisone).
Les antibiotiques à large spectre peuvent renforcer les effets de l'acénocoumarol en réduisant la flore intestinale qui produit la vitamine K.
Les médicaments suivants peuvent diminuer l'effet anticoagulant de l'acénocoumarol :
Aminoglutéthimide, médicaments antinéoplasiques (azathioprine, 6-mercaptopurine), barbituriques, carbamazépine, cholestyramine (voir rubrique 4.9), inhibiteurs de la protéase du VIH, griséofulvine, contraceptifs oraux, rifampicine et diurétiques thiazidiques, bosentan. souffrant de dysfonctionnement hépatique, devrait limiter la consommation d'alcool.
Effets de l'acénocoumarol sur d'autres médicaments
Lors d'un traitement concomitant par des dérivés de l'hydantoïne (comme la phénytoïne), la concentration sérique d'hydantoïne peut augmenter.Au cours d'un traitement concomitant par des dérivés de sulfonylurée, l'effet hypoglycémiant de ces médicaments peut augmenter.
Interactions avec le CYP450
Certaines isoenzymes du CYP450 sont impliquées dans le métabolisme de l'acénocoumarol.
- Les inhibiteurs du CYP2C9 ont le potentiel d'augmenter l'effet (augmentation de l'INR) de l'acénocoumarol en augmentant l'exposition à l'acénocoumarol.
- Les inducteurs des CYP2C9, 2C19 et/ou 3A4 ont le potentiel de diminuer l'effet (diminution de l'INR) de l'acénocoumarol en diminuant l'exposition à l'acénocoumarol.
Composants alimentaires riches en vitamine K.
Les composants alimentaires riches en vitamine K peuvent antagoniser les effets de l'acénocoumarol.Certaines préparations à base de plantes peuvent provoquer des saignements lorsqu'elles sont prises seules (par exemple, l'ail et le Ginkgo biloba) et peuvent avoir des propriétés anticoagulantes, antiplaquettaires et/ou fibrinolytiques. Ces effets devraient s'ajouter aux effets anticoagulants de SINTROM. À l'inverse, certains produits à base de plantes peuvent diminuer l'effet de SINTROM (par exemple la coenzyme Q10, le millepertuis, le ginseng). Certaines préparations à base de plantes et certains aliments peuvent interagir avec SINTROM par le biais d'interactions avec le CYP450 (p. ex., échinacée, jus de pamplemousse, ginko, hydraste, millepertuis).
La réponse du patient doit être surveillée avec d'autres déterminations de l'INR si une préparation à base de plantes est démarrée ou arrêtée.
Certaines préparations à base de plantes qui peuvent affecter la coagulation sont énumérées ci-dessous à titre de référence, bien que cette liste ne doive pas être considérée comme exhaustive. De nombreuses préparations à base de plantes ont plusieurs noms communs et noms scientifiques. Les noms communs les plus connus des préparations à base de plantes sont donnés ci-dessous.
a Contient des coumarines, possède des propriétés antiplaquettaires et peut avoir des propriétés coagulantes en raison de la teneur possible en vitamine K.
b Contient des coumarines et des salicylates.
c Contient des coumarines et possède des propriétés fibrinolytiques.
d Contient des coumarines et possède des propriétés antiplaquettaires.
e Il a des propriétés antiplaquettaires et fibrinolytiques.
millepertuis (Hypericum perforatum)
L'efficacité thérapeutique de l'acénocoumarol pourrait être diminuée par l'administration simultanée de préparations à base de millepertuis (Hypericum perforatum) en raison de l'induction des enzymes responsables du métabolisme des médicaments par ces préparations qui ne doivent donc pas être administrées. en association avec l'acénocoumarol. L'effet d'induction peut persister pendant au moins 2 semaines après l'arrêt du traitement avec les produits Hypericum perforatum. Si un patient prend des produits Hypericum perforatum en concomitance avec l'acénocoumarol, les valeurs de l'INR doivent être surveillées et le traitement avec ce dernier doit être interrompu.Surveiller de près les valeurs de l'INR, car elles peuvent augmenter après l'arrêt d'Hypericum perforatum. La posologie de l'acénocoumarol peut devoir être ajustée.
Avertissements Il est important de savoir que :
Fertilité, grossesse et allaitement
Demandez conseil à votre médecin ou à votre pharmacien avant de prendre tout médicament.
Grossesse
Sintrom, comme d'autres dérivés de la coumarine, peut être associé à des malformations congénitales de l'embryon. Sintrom est donc contre-indiqué chez les femmes enceintes (voir "Contre-indications") ou chez celles susceptibles de devenir enceintes. Les femmes en âge de procréer doivent adopter des mesures contraceptives efficaces. pendant le traitement. avec Sintrom.
L'heure du repas
Sintrom passe dans le lait maternel, les quantités sont faibles et limitées. La décision d'allaiter doit être considérée avec prudence et peut inclure des tests de coagulation et une évaluation du statut en vitamine K chez les nourrissons avant de conseiller à la femme d'allaiter. Les femmes qui allaitent et qui sont traitées par Sintrom doivent être étroitement surveillées pour s'assurer que les valeurs recommandées de PT / INR ne sont pas dépassées. Lors de l'allaitement, le nouveau-né doit recevoir 1 mg de vitamine K1 par semaine à titre prophylactique.
La fertilité
Il n'y a pas de données disponibles sur l'utilisation de Sintrom et ses effets sur la fertilité humaine.
Effets sur l'aptitude à conduire des véhicules et à utiliser des machines
Sintrom n'a aucune influence connue sur l'aptitude à conduire des véhicules et à utiliser des machines.Il est toutefois recommandé aux patients de se munir d'un certificat de traitement anticoagulant en cours pour informer les secouristes en cas d'accident corporel.
Informations importantes sur certains ingrédients
Sintrom contient du lactose. Si votre médecin vous a dit que vous aviez une intolérance à certains sucres, contactez votre médecin avant de prendre ce médicament.
Posologie et mode d'utilisation Comment utiliser Sintrom : Posologie
Les effets indésirables peuvent être minimisés en utilisant la dose efficace la plus faible pendant la durée de traitement la plus courte possible nécessaire pour contrôler les symptômes (voir « Précautions d'emploi »).
Dosage
Population générale La sensibilité aux anticoagulants varie d'un patient à l'autre et peut également fluctuer au cours du traitement.
Par conséquent, il est essentiel d'effectuer des analyses régulières du temps de Quick (TP) / International Normalized Ratio (INR) et d'ajuster la posologie en fonction des résultats fournis par ces analyses. Si cela n'est pas possible, Sintrom ne doit pas être utilisé.
La posologie quotidienne doit toujours être prescrite en une seule dose. Comparez également les « Précautions d'emploi » et les « Interactions » pour adapter la posologie aux différentes conditions cliniques.
Sintrom est disponible sous forme de comprimés à 1 et 4 mg. Pour la prise de faibles doses, il est recommandé d'utiliser les comprimés à 1 mg qui permettent une plus grande précision de dosage.
Posologie initiale
La posologie de Sintrom doit être individualisée.
La dose initiale habituelle de Sintrom est comprise entre 2 mg/jour et 4 mg/jour sans dose de charge si les valeurs PT/INR avant l'instauration du traitement sont dans la plage normale.Le traitement peut également être initié avec une dose de charge, habituellement 6 mg le premier jour suivis de 4 mg le deuxième jour.
Si les valeurs PT / INR sont initialement en dehors de la plage normale, le traitement doit être initié avec prudence.
Les patients âgés (≥ 65 ans), les patients atteints d'une maladie du foie ou d'insuffisance cardiaque sévère avec congestion hépatique, ou les patients dénutris peuvent nécessiter des doses plus faibles en début de traitement et pendant la période d'entretien (voir « Précautions d'emploi »).
À partir de la deuxième ou de la troisième dose de Sintrom et jusqu'à ce que l'état de coagulation se soit stabilisé dans la plage cible, la mesure du PT / INR doit être effectuée quotidiennement. L'intervalle entre les tests peut être prolongé par la suite, en fonction de la stabilité des résultats PT / INR Il est recommandé de toujours prélever les échantillons pour les tests de laboratoire à la même heure de la journée.
Traitement d'entretien et analyse de la coagulation
La dose d'entretien varie d'un patient à l'autre et sa pertinence doit être vérifiée individuellement sur la base des valeurs PT / INR. Les valeurs PT/INR doivent être prises à intervalles réguliers, c'est-à-dire au moins une fois par mois.
La dose d'entretien est normalement positionnée entre 1 et 8 mg/jour en fonction du patient, de la maladie sous-jacente, de l'indication clinique et de l'intensité d'anticoagulation souhaitée.
Sur la base de l'indication clinique, l'intensité optimale de l'anticoagulation ou la plage cible se trouve généralement à des valeurs INR comprises entre 2,0 et 3,5 (voir tableau 1). Dans certains cas, des valeurs INR plus élevées, jusqu'à 4,5, peuvent être nécessaires.
Tableau 1 - INR * recommandé pour le traitement anticoagulant oral
* Le temps de Quick (TP), qui reflète la réduction des facteurs de coagulation dépendants de la vitamine K VII, X et II, dépend de la réactivité de la thromboplastine utilisée pour le test TP. La capacité de réponse de la thromboplastine locale respective par rapport aux préparations internationales de référence de l'Organisation mondiale de la santé est exprimée par l'indice international de sensibilité (ISI).
L'International Normalized Ratio (INR) a été introduit afin de standardiser le PT. L'INR est le rapport entre le PT du plasma anticoagulé du patient et le PT d'un plasma normal, en utilisant la même thromboplastine dans le même système de test augmenté à la puissance de la valeur définie par l'indice international de sensibilité.
Arrêt du traitement
Le traitement par Sintrom peut généralement être arrêté sans qu'il soit nécessaire de réduire progressivement le médicament. Cependant, il a été observé que dans des cas extrêmement rares et chez certains patients à haut risque (par exemple après un infarctus du myocarde), une « hypercoagulabilité rebond » peut survenir. Chez ces patients, l'arrêt du traitement anticoagulant doit être progressif.
Dose oubliée
L'effet anticoagulant de Sintrom persiste pendant plus de 24 heures. Si le patient oublie de prendre la dose prescrite de Sintrom à l'heure prévue, la dose doit être prise dès que possible dans la même journée. Le patient ne doit pas prendre la dose. dose oubliée en doublant la dose quotidienne pour compenser les doses oubliées, mais vous devez contacter votre médecin.
Conversion de l'héparine
Dans les situations cliniques nécessitant une anticoagulation rapide, un traitement initial par héparine est préférable, car l'effet anticoagulant de Sintrom n'est pas immédiat. La conversion à Sintrom peut commencer en même temps que l'héparine ou peut être différée en fonction de la situation clinique. Afin d'assurer la poursuite de l'anticoagulation, il est conseillé de poursuivre le traitement par héparine à pleine dose pendant au moins 4 jours après le début du traitement par Sintrom et de poursuivre le traitement par héparine jusqu'à ce que l'INR soit dans la plage cible pendant au moins deux jours consécutifs. Une surveillance étroite de l'anticoagulation est nécessaire pendant la phase de transition.
Traitement pendant le traitement dentaire et la chirurgie
Les patients traités par Sintrom, subissant des procédures chirurgicales ou invasives, nécessitent une surveillance étroite de leur état de coagulation. Dans certaines conditions, par exemple lorsque le site opératoire est limité et accessible pour permettre une utilisation efficace des procédures hémostatiques locales, des procédures dentaires et chirurgicales mineures peuvent être réalisées pendant la poursuite de l'anticoagulation sans risque de saignement. La décision d'arrêter Sintrom, même pour une courte période, doit soigneusement prendre en compte les risques et les avantages individuels. L'introduction d'un traitement de transition anticoagulant - par exemple avec de l'héparine - doit être basée sur un examen attentif des risques attendus de thromboembolie et d'hémorragie.
Populations particulières
Insuffisance rénale
En raison du risque accru de saignement, l'utilisation de Sintrom est contre-indiquée chez les patients présentant une insuffisance rénale sévère. Chez les patients présentant une insuffisance rénale légère à modérée, des précautions doivent être prises (voir également « Contre-indications » et « Précautions d'emploi »).
Insuffisance hépatique
En raison du risque accru de saignement, l'utilisation de Sintrom est contre-indiquée chez les patients présentant une insuffisance hépatique sévère. Chez les patients présentant une insuffisance hépatique légère à modérée, des précautions doivent être prises (voir également « Contre-indications » et « Précautions d'emploi »).
Population pédiatrique
Les informations issues des essais cliniques contrôlés sur l'utilisation chez les enfants sont insuffisantes.La sécurité et l'efficacité de SINTROM chez les enfants et les adolescents de moins de 18 ans n'ont pas été établies.
Personnes âgées (≥ 65 ans)
L'utilisation chez les patients âgés peut nécessiter des doses initiales et d'entretien plus faibles. Une attention particulière et une surveillance plus fréquente du temps de Quick et de l'INR sont recommandées (voir également « Précautions d'emploi »).
Mode d'administration
La dose quotidienne doit toujours être prise à la même heure de la journée. Le comprimé doit être avalé entier avec un verre d'eau.
Surdosage Que faire si vous avez pris trop de Sintrom
Si les doses uniques, même très élevées, ne sont généralement pas dangereuses, les manifestations cliniques d'un surdosage peuvent survenir lors d'une utilisation prolongée de doses quotidiennes supérieures à celles nécessaires au traitement.
Signes et symptômes
La sensibilité de chaque patient aux anticoagulants oraux, l'étendue du surdosage et la durée du traitement affectent la manifestation et la gravité des effets.
Les hémorragies dans divers organes sont la manifestation la plus importante du tableau clinique. Ils peuvent prendre la forme de saignements cutanés (80%), hématurie (52%), épistaxis, hématémèse, saignements gastro-intestinaux, saignements vaginaux, saignements articulaires, hématomes, saignements gingivaux.
Les symptômes supplémentaires incluent la tachycardie, l'hypotension, les troubles circulatoires dus à la perte de sang, les nausées, les vomissements, la diarrhée et les douleurs abdominales.
Les tests de laboratoire révèlent une valeur PT / INR extrêmement élevée, une prolongation prononcée de la recalcification ou du temps de Quick et des modifications de la gamma-carboxylation des facteurs II, VII, IX et X.
Traitement
La nécessité ou l'opportunité d'un traitement par sirop d'ipéca, lavage gastrique en plus du charbon activé et administration de cholestyramine est controversée.Le bénéfice de ces traitements par rapport au risque hémorragique doit être pesé chez chaque patient.
Mesures d'urgence et de soutien
En cas d'hémorragie sévère, quel que soit le niveau d'INR, les facteurs de coagulation peuvent être restaurés à des valeurs normales par administration de sang total frais ou de concentrés de plasma congelé, de concentré de complexe prothrombique ou de facteur VIIa recombinant supplémenté en vitamine K1.
Antidote
La vitamine K1 (phytoménadione) peut s'opposer à l'effet inhibiteur de Sintrom sur la gamma-carboxylation hépatique des facteurs de coagulation dépendants de la vitamine K en 3 à 5 heures.
En cas de saignement cliniquement insignifiant (INR < 4,5), tel qu'une épistaxis courte ou de petits hématomes isolés, une réduction temporaire de la posologie ou l'omission d'une dose de Sintrom est souvent suffisante.
En cas d'INR élevé (INR 4,5-9) avec saignement insignifiant, omettre une ou deux doses de Sintrom et administrer 1-2,5 mg de vitamine K1 par voie orale, en particulier chez les patients présentant un risque accru de saignement.
En cas d'INR élevé (INR> 9) avec saignement non significatif, interrompre le traitement par Sintrom et administrer 2,5 à 5 mg de vitamine K1 par voie orale. En cas de saignement modéré à sévère, Sintrom peut être ré-administré lorsque l'INR est dans la plage cible.
En cas d'ingestion/prise accidentelle d'une dose excessive de Sintrom, informez immédiatement votre médecin ou rendez-vous à l'hôpital le plus proche.
Si vous avez des questions sur l'utilisation de Sintrom, demandez à votre médecin ou votre pharmacien
Effets secondaires Quels sont les effets secondaires de Sintrom
Comme tous les médicaments, Sintrom est susceptible d'avoir des effets indésirables, bien que tout le monde n'y soit pas sujet.
Les effets indésirables (tableau 2) sont répertoriés par classes de systèmes d'organes dans MedDRA. Au sein de chaque classe de systèmes d'organes, les effets indésirables sont classés par fréquence, les effets les plus fréquents en premier. Dans chaque groupe de fréquence, les effets indésirables sont présentés par ordre décroissant de gravité. De plus, pour chaque effet indésirable, la catégorie de fréquence correspondante est également fournie selon la convention suivante (CIOMS III) : très fréquent (≥ 1/10) ; fréquent (≥ 1/100 - < 1/10), peu fréquent (≥ 1 / 1 000 - < 1/100) ; rare (≥ 1 / 10 000 - < 1 / 1 000) ; très rare (<1/10 000), fréquence indéterminée (ne peut être estimée sur la base des données disponibles).
Hémorragies
Les saignements dans différentes parties du corps sont les complications les plus fréquemment rapportées avec Sintrom et ont été liés à la posologie, à l'âge du patient et à la nature de la maladie sous-jacente (mais pas à la durée du traitement).
Tableau 2
* normalement associé à un déficit congénital en protéine C ou en son cofacteur protéine S
Le respect des instructions contenues dans la notice réduit le risque d'effets indésirables.
Déclaration des effets secondaires
Si vous ressentez un quelconque effet indésirable, parlez-en à votre médecin ou votre pharmacien, y compris tout effet indésirable éventuel non mentionné dans cette notice. Les effets indésirables peuvent également être signalés directement via le système national de notification à l'adresse www.agenziafarmaco.gov.it/it/responsabili. En signalant les effets indésirables, vous pouvez contribuer à fournir plus d'informations sur la sécurité de ce médicament.
Expiration et conservation
Expiration : voir la date d'expiration imprimée sur l'emballage.
La date de péremption fait référence au produit dans un emballage intact, correctement stocké.
Attention : ne pas utiliser le médicament après la date de péremption indiquée sur l'emballage.
Les médicaments ne doivent pas être jetés au tout à l'égout ou avec les ordures ménagères.Demandez à votre pharmacien comment jeter les médicaments que vous n'utilisez plus.Cela contribuera à protéger l'environnement.
Gardez ce médicament hors de la vue et de la portée des enfants.
Composition et forme pharmaceutique
Comprimés de Sintrom 1 mg
Chaque comprimé contient : Ingrédient actif : 1 mg d'acénocoumarol. Excipients : silice colloïdale anhydre ; hypromellose; lactose monohydraté; stéarate de magnésium; fécule de maïs; talc.
Sintrom 4 mg comprimés
Chaque comprimé contient : Ingrédient actif : 4 mg d'acénocoumarol. Excipients : silice colloïdale anhydre ; lactose monohydraté; stéarate de magnésium; fécule de maïs; amidon de maïs prégélatinisé.
Forme et contenu pharmaceutiques
Comprimés Sintrom 1 mg : 20 et 100 comprimés. Sintrom 4 mg comprimés : 20 comprimés quadrisécables.
Notice d'emballage source : AIFA (Agence italienne des médicaments). Contenu publié en janvier 2016. Les informations présentes peuvent ne pas être à jour.
Pour avoir accès à la version la plus à jour, il est conseillé d'accéder au site Internet de l'AIFA (Agence Italienne du Médicament). Avis de non-responsabilité et informations utiles.
01.0 DÉNOMINATION DU MÉDICAMENT
COMPRIMÉS SINTROM
02.0 COMPOSITION QUALITATIVE ET QUANTITATIVE
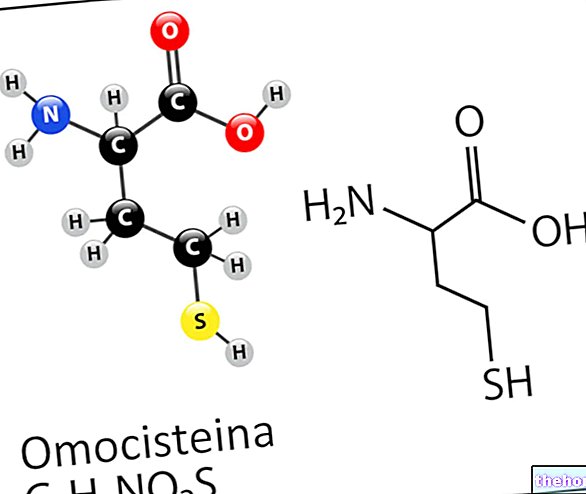
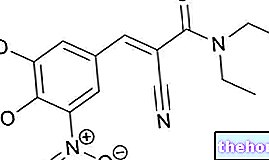
Ingrédient actif : 3- [α- (4-nitrophényl) -β-acétyl-éthyl] -4-hydroxycoumarine (= acénocoumarol) sous forme de mélange racémique. L'acénocoumarol est un dérivé de la 4-hydroxycoumarine.
Excipients à effet notoire : lactose monohydraté
Pour la liste des excipients voir rubrique 6.1
03.0 FORME PHARMACEUTIQUE
Comprimés à 1 mg
Blanc, rond, plat, avec bords légèrement biseautés, lettres CG en relief d'un côté, lettres AA en relief de l'autre côté.
Comprimés de 4 mg
Blanc, rond, plat, à bords légèrement biseautés, lettres CG en relief d'un côté, gravure en croix de l'autre côté avec la lettre A en relief sur chaque cadran.
04.0 INFORMATIONS CLINIQUES
04.1 Indications thérapeutiques
Traitement et prévention des maladies thromboemboliques.
04.2 Posologie et mode d'administration
Dosage
Population générale
La sensibilité aux anticoagulants varie d'un patient à l'autre et peut également fluctuer au cours du traitement.
Par conséquent, il est essentiel d'effectuer des analyses régulières du temps de Quick (TP) / International Normalized Ratio (INR) et d'ajuster la posologie en fonction des résultats fournis par ces analyses. Si cela n'est pas possible, Sintrom ne doit pas être utilisé.
La posologie quotidienne doit toujours être prescrite en une seule dose.
Pour l'adaptation de la posologie à diverses conditions cliniques, voir rubriques 4.4 et 4.5.
Sintrom est disponible sous forme de comprimés à 1 et 4 mg. Pour la prise de faibles doses, il est recommandé d'utiliser les comprimés à 1 mg qui permettent une plus grande précision de dosage.
Posologie initiale
La posologie de Sintrom doit être individualisée.
La dose initiale habituelle de Sintrom est comprise entre 2 mg/jour et 4 mg/jour sans dose de charge si les valeurs PT/INR avant l'instauration du traitement sont dans la plage normale.Le traitement peut également être initié avec une dose de charge, habituellement 6 mg le premier jour suivis de 4 mg le deuxième jour.
Si les valeurs initiales PT / INR sont en dehors de la plage normale, le traitement doit être démarré avec prudence.
Les patients âgés (≥ 65 ans), les patients atteints d'une maladie hépatique ou d'insuffisance cardiaque sévère avec congestion hépatique, ou les patients dénutris peuvent nécessiter des doses plus faibles au début du traitement et pendant la période d'entretien (voir rubrique 4.4).
À partir de la deuxième ou de la troisième dose de Sintrom et jusqu'à ce que l'état de coagulation se soit stabilisé dans la plage cible, la mesure du PT / INR doit être effectuée quotidiennement. L'intervalle entre les tests peut être prolongé par la suite, en fonction de la stabilité des résultats PT / INR Il est recommandé de toujours prélever les échantillons pour les tests de laboratoire à la même heure de la journée.
Traitement d'entretien et analyse de la coagulation
La dose d'entretien varie d'un patient à l'autre et sa pertinence doit être vérifiée individuellement sur la base des valeurs PT / INR. Les valeurs PT/INR doivent être prises à intervalles réguliers, c'est-à-dire au moins une fois par mois.
La dose d'entretien est normalement positionnée entre 1 et 8 mg/jour en fonction du patient, de la maladie sous-jacente, de l'indication clinique et de l'intensité d'anticoagulation souhaitée.
Sur la base de l'indication clinique, l'intensité optimale de l'anticoagulation ou la plage cible se trouve généralement à des valeurs INR comprises entre 2,0 et 3,5 (voir tableau 1). Dans certains cas, des valeurs INR plus élevées, jusqu'à 4,5, peuvent être nécessaires.
Tableau 1 - INR * recommandé pour le traitement anticoagulant oral
* Le temps de Quick (TP), qui reflète la réduction des facteurs de coagulation dépendants de la vitamine K VII, X et II, dépend de la réactivité de la thromboplastine utilisée pour le test TP. La capacité de réponse de la thromboplastine locale respective par rapport aux préparations internationales de référence de l'Organisation mondiale de la santé est exprimée par l'indice international de sensibilité (ISI).
L'International Normalized Ratio (INR) a été introduit afin de standardiser le PT. L'INR est le rapport entre le PT du plasma anticoagulé du patient et le PT d'un plasma normal, en utilisant la même thromboplastine dans le même système de test augmenté à la puissance de la valeur définie par l'indice international de sensibilité.
Arrêt du traitement
Le traitement par Sintrom peut généralement être arrêté sans qu'il soit nécessaire de réduire progressivement le médicament.
Cependant, il a été observé que dans des cas extrêmement rares et chez certains patients à haut risque (par exemple après un infarctus du myocarde), une « hypercoagulabilité rebond » peut survenir. Chez ces patients, l'arrêt du traitement anticoagulant doit être progressif.
Dose oubliée
L'effet anticoagulant de Sintrom persiste pendant plus de 24 heures. Si le patient oublie de prendre la dose prescrite de Sintrom à l'heure prévue, la dose doit être prise dès que possible dans la même journée. Le patient ne doit pas prendre la dose. dose oubliée en doublant la dose quotidienne pour compenser les doses oubliées, mais vous devez contacter votre médecin.
Conversion de l'héparine
Dans les situations cliniques nécessitant une anticoagulation rapide, un traitement initial par héparine est préférable, car l'effet anticoagulant de Sintrom n'est pas immédiat. La conversion à Sintrom peut commencer en même temps que l'héparine ou peut être différée en fonction de la situation clinique. Afin d'assurer la poursuite de l'anticoagulation, il est conseillé de poursuivre le traitement par héparine à pleine dose pendant au moins 4 jours après le début du traitement par Sintrom et de poursuivre le traitement par héparine jusqu'à ce que l'INR soit dans la plage cible pendant au moins deux jours consécutifs. Une surveillance étroite de l'anticoagulation est nécessaire pendant la phase de transition.
Traitement pendant le traitement dentaire et la chirurgie
Les patients traités par Sintrom, subissant des procédures chirurgicales ou invasives, nécessitent une surveillance étroite de leur état de coagulation. Dans certaines conditions, par exemple lorsque le site opératoire est limité et accessible pour permettre une utilisation efficace des procédures hémostatiques locales, des procédures dentaires et chirurgicales mineures peuvent être réalisées pendant la poursuite de l'anticoagulation sans risque de saignement. La décision d'arrêter Sintrom, même pour une courte période, doit soigneusement prendre en compte les risques et les avantages individuels. L'introduction d'une thérapie
le pontage - par exemple avec l'héparine - doit être basé sur un examen attentif des risques attendus de thromboembolie et d'hémorragie.
Populations particulières
Insuffisance rénale
En raison du risque accru de saignement, l'utilisation de Sintrom est contre-indiquée chez les patients présentant une insuffisance rénale sévère. Chez les patients présentant une insuffisance rénale légère à modérée, des précautions doivent être prises (voir rubriques 4.3, 4.4 et 5.1).
Insuffisance hépatique
En raison du risque accru de saignement, l'utilisation de Sintrom est contre-indiquée chez les patients présentant une insuffisance hépatique sévère. Chez les patients présentant une insuffisance hépatique légère à modérée, des précautions doivent être prises (voir rubriques 4.3, 4.4 et 5.1).
Population pédiatrique
Il n'y a pas suffisamment d'informations provenant d'essais cliniques contrôlés sur l'utilisation chez les enfants.
La sécurité et l'efficacité de SINTROM chez les enfants et les adolescents de moins de 18 ans n'ont pas été établies.
Personnes âgées (≥ 65 ans)
L'utilisation chez les patients âgés peut nécessiter des doses initiales et d'entretien plus faibles.Une attention particulière et une surveillance plus fréquente du temps de Quick et de l'INR sont recommandées (voir rubrique 4.4).
Mode d'administration
La dose quotidienne doit toujours être prise à la même heure de la journée. Le comprimé doit être avalé entier avec un verre d'eau.
04.3 Contre-indications
• Hypersensibilité à la substance active, aux dérivés coumariniques apparentés ou à l'un des excipients mentionnés à la rubrique 6.1.
• Grossesse.
• Chez les femmes en âge de procréer qui n'utilisent pas de mesures contraceptives (voir rubrique 4.6 « Fécondité, grossesse et allaitement »).
• Patients incapables de coopérer et non supervisés avec un risque élevé associé de non-observance du traitement
Sintrom est également contre-indiqué dans tous les états pathologiques dans lesquels le risque de saignement est supérieur au bénéfice clinique possible, par exemple :
• diathèse hémorragique et/ou dyscrasie sanguine ;
• immédiatement avant ou après une intervention chirurgicale du système nerveux central, ainsi que des opérations ophtalmologiques et des interventions chirurgicales traumatisantes avec exposition étendue des tissus ;
• ulcère gastroduodénal ou en présence d'hémorragie du tractus gastro-intestinal, du tractus urogénital ou de l'appareil respiratoire, ainsi qu'en cas d'hémorragies cérébrovasculaires, de péricardite aiguë et d'épanchement péricardique, et d'endocardite bactérienne ;
• hypertension sévère ;
• insuffisance hépatique sévère (voir rubrique 4.2 « Posologie et mode d'administration ») ;
• insuffisance rénale sévère (voir rubrique 4.2 « Posologie et mode d'administration ») ;
• augmentation de l'activité fibrinolytique comme après des opérations sur les poumons, la prostate, l'utérus et dans la pancréatite aiguë ;
• insuffisance circulatoire sévère avec stase hépatique.
Les préparations d'Hypericum perforatum ne doivent pas être prises en même temps que des médicaments contenant de l'acénocoumarol, en raison du risque de diminution des concentrations plasmatiques et de diminution de l'efficacité thérapeutique de l'acénocoumarol (voir rubrique 4.5).
04.4 Mises en garde spéciales et précautions d'emploi appropriées
L'administration de Sintrom pendant l'allaitement nécessite des précautions (voir rubrique 4.6).
Insuffisance hépatique
Chez les patients présentant une insuffisance hépatique légère à modérée, des précautions doivent être prises car la synthèse des facteurs de coagulation peut également être altérée ou il peut y avoir un dysfonctionnement plaquettaire sous-jacent (voir également rubriques 4.2 et 5.1). L'utilisation chez les patients présentant une insuffisance hépatique sévère est contre-indiquée (voir rubrique 4.3).
Insuffisance rénale
En raison de la possibilité d'accumulation de métabolites en présence d'insuffisance rénale, des précautions doivent être prises chez les patients présentant une insuffisance rénale légère à modérée (voir rubriques 4.2 et 5.1). L'utilisation chez les patients présentant une insuffisance rénale sévère est contre-indiquée (voir rubrique 4.3).
Insuffisance cardiaque
En cas d'insuffisance cardiaque sévère, un schéma posologique réduit et une surveillance biologique fréquente doivent être utilisés, car l'activation ou la gamma-carboxylation des facteurs de coagulation peut être réduite en cas de congestion hépatique (voir rubrique 4.2). peut être nécessaire d'augmenter la dose.
Maladies hématologiques
Une prudence particulière doit être exercée chez les patients présentant un déficit connu ou suspecté en protéine C ou en protéine S car l'administration d'acénocoumarol a été associée à une nécrose tissulaire (voir rubrique 4.8).
Population pédiatrique
Aucune étude adéquate et bien contrôlée n'a été menée dans la population pédiatrique et la dose optimale, la sécurité et l'efficacité dans cette population ne sont pas connues.
Utilisation chez les personnes âgées
Chez les patients âgés (≥ 65 ans), une attention particulière et une surveillance plus fréquente du temps de Quick et de l'INR sont recommandées (voir rubrique 4.2).
Une surveillance médicale étroite est requise dans les cas où des conditions ou des maladies peuvent réduire la liaison aux protéines de Sintrom, par exemple, la thyréotoxicose, le cancer, les maladies rénales, les infections et les inflammations.
Les troubles de l'absorption gastro-intestinale peuvent altérer l'effet anticoagulant de Sintrom.
Lors d'un traitement par anticoagulants, les injections intramusculaires peuvent provoquer des hématomes et sont donc contre-indiquées. Les injections intraveineuses et sous-cutanées n'entraînent pas de telles complications.
Traitement continu des opérations diagnostiques, dentaires et chirurgicales
Certaines procédures diagnostiques dentaires ou chirurgicales (angiographie, ponction lombaire) peuvent nécessiter une « interruption ou une modification de la dose du traitement par SINTROM. Les risques et les avantages de l'arrêt du traitement par SINTROM, même pour de courtes périodes, doivent être pris en compte. L" INR doit être déterminé immédiatement avant chaque procédure. Chez les patients subissant des procédures mini-invasives qui doivent être anticoagulés avant, pendant ou immédiatement après de telles procédures, un ajustement de la dose de SINTROM afin de maintenir l'INR au niveau le plus bas de la plage thérapeutique peut permettre en toute sécurité de maintenir le maintien. » anticoagulant.
Pendant le traitement par Sintrom, il est recommandé aux patients de porter une carte qui, en cas d'accident, avertit du traitement anticoagulant en cours.
Pharmacogénétique
La variabilité génétique notamment en relation avec les gènes codant pour les protéines CYP2C9 et VKORC1 peut influencer significativement la dose d'acénocoumarol nécessaire pour obtenir l'effet clinique recherché.Si une association avec ces polymorphismes est connue, une extrême prudence doit être exercée (voir également paragraphe 5.2).
Informations importantes sur certains ingrédients
Sintrom contient du lactose. Les patients présentant des problèmes héréditaires rares d'intolérance au galactose, de déficit en lactase de Lapp ou de malabsorption du glucose et du galactose ne doivent pas prendre ce médicament.
04.5 Interactions avec d'autres médicaments et autres formes d'interactions
Il existe de nombreuses interactions possibles entre les coumarines et d'autres médicaments. Les mécanismes impliqués dans de telles interactions comprennent : des perturbations de l'absorption, de l'inhibition ou de l'induction du système métabolique enzymatique (principalement le CYP2C9, voir également rubrique 5) et une disponibilité réduite de la vitamine K nécessaire à la gamma-carboxylation des facteurs du complexe prothrombique. Il est important de noter que certains médicaments peuvent interagir avec plus d'un mécanisme. Chaque thérapie peut comporter un risque d'interactions bien que toutes les interactions ne soient pas significatives. D'où la nécessité d'une surveillance attentive et de tests de coagulation fréquents (généralement deux fois par semaine) lorsqu'un médicament est prescrit pour la première fois en association avec Sintrom ou si un médicament concomitant est interrompu.
Interactions pour lesquelles l'utilisation concomitante n'est pas recommandée
Effets d'autres médicaments sur l'acénocoumarol
Les médicaments suivants potentialisent l'effet anticoagulant de l'acénocoumarol et/ou altèrent l'hémostase et augmentent ainsi le risque hémorragique :
• Anticoagulants (concernant l'utilisation de l'héparine dans les situations nécessitant une anticoagulation rapide, voir rubrique 4.2)
• Agents antiplaquettaires
• Thrombolytiques
• Anti-inflammatoires non stéroïdiens (AINS)
• Inhibiteurs de la recapture de la sérotonine
L'utilisation de Sintrom associé à ces substances est donc déconseillée.En cas d'utilisation en association avec ces médicaments, des tests de coagulation doivent être réalisés plus fréquemment.
Interactions à considérer
Les médicaments suivants peuvent potentialiser l'effet anticoagulant de l'acénocoumarol :
Allopurinol, stéroïdes anabolisants, androgènes, agents antiarythmiques (tels que amiodarone, quinidine, propafénone), antibactériens (tels que clindamycine, pénicillines, céphalosporines de deuxième et troisième génération, chloramphénicol, macrolides, fluoroquinolones, néomycine, tétracyclines, , dérivés de l'imidazole (par exemple métronidazole et, également en cas d'administration locale, miconazole), paracétamol, statines, sulfamides, y compris cotrimoxazole (= sulfaméthoxazole + triméthoprime), sulfonylurées (telles que tolbutamide et chlorpropamide), hormones), tamoxifène, tramadol, proton inhibiteurs de la pompe, agents procinétiques (cisapride, antiacides (hydroxyde de magnésium) et viloxazine, 5-fluorouracile et analogues, vitamine E, corticostéroïdes (tels que dexaméthasone, méthylprednisolone, prednisone).
Les antibiotiques à large spectre peuvent renforcer les effets de l'acénocoumarol en réduisant la flore intestinale qui produit la vitamine K.
Les médicaments suivants peuvent diminuer l'effet anticoagulant de l'acénocoumarol : Aminoglutéthymide, médicaments antinéoplasiques (azathioprine, 6-mercaptopurine), barbituriques, carbamazépine, cholestyramine (voir rubrique 4.9), inhibiteurs de la protéase du VIH, griséofulvine, contraceptifs oraux, tampicine diurétiques, bosentan.
Étant donné que ni la gravité ni les premiers symptômes des interactions ne peuvent être prédits, les patients prenant Sintrom, en particulier ceux présentant un dysfonctionnement hépatique, doivent limiter leur consommation d'alcool.
Effets de l'acénocoumarol sur d'autres médicaments
Lors d'un traitement concomitant par des dérivés de l'hydantoïne (tels que la phénytoïne), la concentration sérique d'hydantoïne peut augmenter.
Lors d'un traitement concomitant par des dérivés de sulfonylurée, l'effet hypoglycémiant de ces médicaments peut augmenter.
Interactions avec le CYP450
Certaines isoenzymes du CYP450 sont impliquées dans le métabolisme de l'acénocoumarol.
• Les inhibiteurs du CYP2C9 ont le potentiel d'augmenter l'effet (augmentation de l'INR) de l'acénocoumarol en augmentant l'exposition à l'acénocoumarol.
• Les inducteurs des CYP2C9, 2C19 et/ou 3A4 ont le potentiel de diminuer l'effet (INR inférieur) de l'acénocoumarol en diminuant l'exposition à l'acénocoumarol.
Composants alimentaires riches en vitamine K.
Les composants alimentaires riches en vitamine K peuvent antagoniser les effets de l'acénocoumarol.
Certaines préparations à base de plantes peuvent provoquer des saignements lorsqu'elles sont prises seules (par exemple, l'ail et le Ginkgo biloba) et peuvent avoir des propriétés anticoagulantes, antiplaquettaires et/ou fibrinolytiques. Ces effets devraient s'ajouter aux effets anticoagulants de SINTROM. peut diminuer l'effet de SINTROM (par exemple, coenzyme Q10, millepertuis, ginseng).Certaines préparations à base de plantes et certains aliments peuvent interagir avec SINTROM par le biais d'interactions avec le CYP450 (par exemple, échinacée, jus de pamplemousse, ginko, hydraste, millepertuis) .
La réponse du patient doit être surveillée avec d'autres déterminations de l'INR si une préparation à base de plantes est démarrée ou arrêtée.
Certaines préparations à base de plantes qui peuvent affecter la coagulation sont énumérées ci-dessous à titre de référence, bien que cette liste ne doive pas être considérée comme exhaustive. De nombreuses préparations à base de plantes ont plusieurs noms communs et noms scientifiques. Les noms communs les plus connus des préparations à base de plantes sont donnés ci-dessous.
a Contient des coumarines, possède des propriétés antiplaquettaires et peut avoir des propriétés coagulantes en raison de la teneur possible en vitamine K.
b Contient des coumarines et des salicylates.
c Contient des coumarines et possède des propriétés fibrinolytiques.
d Contient des coumarines et possède des propriétés antiplaquettaires.
e Il a des propriétés antiplaquettaires et fibrinolytiques.
millepertuis (Hypericum perforatum)
L'efficacité thérapeutique de l'acénocoumarol pourrait être diminuée par l'administration simultanée de préparations à base de millepertuis (Hypericum perforatum) en raison de l'induction des enzymes responsables du métabolisme des médicaments par ces préparations qui ne doivent donc pas être administrées. en association avec l'acénocoumarol. L'effet d'induction peut persister pendant au moins 2 semaines après l'arrêt du traitement avec les produits Hypericum perforatum.
Si un patient prend des produits Hypericum perforatum en concomitance avec l'acénocoumarol, les valeurs de l'INR doivent être surveillées et le traitement avec ce dernier doit être interrompu.
Surveiller de près les valeurs de l'INR, car elles peuvent augmenter après l'arrêt d'Hypericum perforatum. La posologie de l'acénocoumarol peut devoir être ajustée.
04.6 Grossesse et allaitement
Grossesse
Sintrom, comme d'autres dérivés de la coumarine, peut être associé à des malformations congénitales de l'embryon. Sintrom est donc contre-indiqué chez les femmes enceintes (voir rubrique 4.3) ou chez les femmes susceptibles de devenir enceintes. Les femmes en âge de procréer doivent utiliser des mesures contraceptives efficaces pendant le traitement par Sintrom.
Grossesse
Sintrom passe dans le lait maternel, les quantités sont limitées. La décision d'allaiter doit être considérée avec prudence et peut inclure des tests de coagulation et une évaluation du statut en vitamine K chez les nourrissons avant de conseiller à la femme d'allaiter. Les femmes qui allaitent et qui sont traitées par Sintrom doivent être étroitement surveillées pour s'assurer que les valeurs recommandées de PT / INR ne sont pas dépassées.
Lors de l'allaitement, le nouveau-né doit recevoir 1 mg de vitamine K1 par semaine à titre prophylactique.
La fertilité
Il n'y a pas de données disponibles sur l'utilisation de Sintrom et ses effets sur la fertilité humaine.
04.7 Effets sur l'aptitude à conduire des véhicules et à utiliser des machines
Sintrom n'a aucune influence connue sur l'aptitude à conduire des véhicules et à utiliser des machines.Il est toutefois recommandé aux patients de se munir d'un certificat de traitement anticoagulant en cours pour informer les secouristes en cas d'accident corporel.
04.8 Effets indésirables
Les effets indésirables (tableau 2) sont répertoriés par classes de systèmes d'organes dans MedDRA. Au sein de chaque classe de systèmes d'organes, les effets indésirables sont classés par fréquence, les effets les plus fréquents en premier. Dans chaque groupe de fréquence, les effets indésirables sont présentés par ordre décroissant de gravité. De plus, pour chaque effet indésirable, la catégorie de fréquence correspondante est également fournie selon la convention suivante (CIOMS III) : très fréquent : (≥ 1/10) ; commun (≥ 1/100 -
Hémorragies
Les saignements dans différentes parties du corps sont les complications les plus fréquemment rapportées avec Sintrom et ont été liés à la dose, à l'âge du patient et à la nature de la maladie sous-jacente (mais pas à la durée du traitement).
Tableau 2
* normalement associé à un déficit congénital en protéine C ou en son cofacteur protéine S
Déclaration des effets indésirables suspectés
La déclaration des effets indésirables suspectés survenant après l'autorisation du médicament est importante car elle permet un suivi continu du rapport bénéfice/risque du médicament. Les professionnels de santé sont invités à déclarer tout effet indésirable suspecté via le système national de déclaration. » adresse https : //www.aifa.gov.it/content/segnalazioni-reazioni-avverse".
04.9 Surdosage
Si les doses uniques, même très élevées, ne sont généralement pas dangereuses, les manifestations cliniques d'un surdosage peuvent survenir lors d'une utilisation prolongée de doses quotidiennes supérieures à celles nécessaires au traitement.
Signes et symptômes
La sensibilité de chaque patient aux anticoagulants oraux, l'étendue du surdosage et la durée du traitement affectent la manifestation et la gravité des effets.
Les hémorragies dans divers organes sont la manifestation la plus importante du tableau clinique. Ils peuvent prendre la forme de saignements cutanés (80%), hématurie (52%), épistaxis, hématémèse, saignements gastro-intestinaux, saignements vaginaux, saignements articulaires, hématomes, saignements gingivaux.
Les symptômes supplémentaires incluent la tachycardie, l'hypotension, les troubles circulatoires dus à la perte de sang, les nausées, les vomissements, la diarrhée et les douleurs abdominales.
Les tests de laboratoire révèlent une valeur PT / INR extrêmement élevée, une prolongation prononcée de la recalcification ou du temps de Quick et des modifications de la gamma-carboxylation des facteurs II, VII, IX et X.
Traitement
La nécessité ou l'opportunité d'un traitement par sirop d'ipéca, lavage gastrique en plus du charbon activé et administration de cholestyramine est controversée.Le bénéfice de ces traitements par rapport au risque hémorragique doit être pesé chez chaque patient.
Mesures d'urgence et de soutien
En cas d'hémorragie sévère, quel que soit le niveau d'INR, les facteurs de coagulation peuvent être restaurés à des valeurs normales par administration de sang total frais ou de concentrés de plasma congelé, de concentré de complexe prothrombique ou de facteur VIIa recombinant supplémenté en vitamine K1.
Antidote
La vitamine K1 (phytoménadione) peut s'opposer à l'effet inhibiteur de Sintrom sur la gamma-carboxylation hépatique des facteurs de coagulation dépendants de la vitamine K en 3 à 5 heures.
En cas de saignement cliniquement insignifiant (INR
En cas d'INR élevé (INR 4,5-9) avec saignement insignifiant, omettre une ou deux doses de Sintrom et administrer 1-2,5 mg de vitamine K1 par voie orale, en particulier chez les patients présentant un risque accru de saignement.
En cas d'INR élevé (INR> 9) avec saignement non significatif, interrompre le traitement par Sintrom et administrer 2,5 à 5 mg de vitamine K1 par voie orale.
S'il existe des signes de saignement important (à n'importe quel niveau d'INR), arrêtez le traitement par Sintrom et injectez 5 à 10 mg de vitamine K1 par voie intraveineuse, très lentement (à un débit ne dépassant pas 1 mg / minute). En cas de saignement, Sintrom peut être ré-administré lorsque l'INR se situe dans la plage préfixée.
05.0 PROPRIÉTÉS PHARMACOLOGIQUES
05.1 Propriétés pharmacodynamiques
Classe pharmacothérapeutique : Antithrombotiques. Antagonistes de la vitamine K.
Code ATC : B01AA07
L'acénocoumarol, la substance active de Sintrom, est un dérivé de la coumarine et agit comme un antagoniste de la vitamine K.Les antagonistes de la vitamine K produisent leur effet anticoagulant par l'inhibition de la vitamine K époxy réductase avec une réduction conséquente de la gamma-carboxylation de certaines molécules d'acide glutamique situées dans différents sites près des deux extrémités des facteurs de coagulation II (prothrombine), VII, IX et X , ainsi que la protéine C ou son cofacteur protéine S. Cette gamma-carboxylation a une relation significative avec l'interaction entre les facteurs de coagulation susmentionnés et les ions calcium. Sans cette réaction, la coagulation du sang ne peut pas commencer.
Sur la base de la posologie initiale, l'acénocoumarol provoque un allongement du TP/INR dans un délai d'environ 36 à 72 heures.À l'arrêt du traitement, le TP/INR revient généralement à la normale après quelques jours.
05.2 Propriétés pharmacocinétiques
Absorption
L'acénocoumarol, un mélange racémique d'énantiomères optiques R (+) et S (-), est rapidement absorbé par voie orale ; au moins 60 % de la dose devient disponible par voie systémique. Après une dose unique de 10 mg, les concentrations plasmatiques maximales sont atteintes de 0,3 ± 0,05 μg/mL en 1 à 3 heures Les concentrations plasmatiques maximales et les aires sous la courbe des concentrations sanguines (ASC) sont proportionnelles à la dose sur une plage de 8 à 16 mg.
Les concentrations plasmatiques d'un patient à l'autre varient de telle sorte qu'aucune corrélation ne peut être établie entre la dose, les concentrations plasmatiques d'acénocoumarol et le taux de prothrombine mesurable.
Distribution
La majeure partie de la dose administrée est distribuée dans la fraction plasmatique du sang, où 98,7 % sont liés aux protéines plasmatiques, principalement à l'albumine. Le volume apparent de distribution est de 0,16-0,18 L/kg par l"R (+) énantiomère et 0,22- 0,34 L/kg pour l'énantiomère S (-).
L'acénocoumarol passe dans le lait maternel, mais seulement en très petites quantités, qui ne peuvent pas être détectées par les méthodes analytiques courantes. Il traverse également la barrière placentaire (voir rubrique 4.6).
Biotransformation / Métabolisme
L'acénocoumarol est largement métabolisé. Les 6- et 7-hydroxylates des deux énantiomères de l'acénocoumarol sont les principaux métabolites et le cytochrome P450 2C9 est le principal catalyseur de la formation de ces 4 métabolites. Le CYP1A2 et le CYP2C19 sont d'autres enzymes impliquées dans le métabolisme. de (R) -acénocoumarol. Par la réduction du groupe cétone, deux métabolites alcooliques différents sont formés. Un métabolite aminé est obtenu par réduction du groupe nitro. Tous ces métabolites sont pharmacologiquement inactifs chez l'homme, alors qu'ils sont actifs dans un modèle animal. La variabilité liée au CYP2C9 représente 14 % de la variabilité interindividuelle de la réponse pharmacodynamique à l'acénocoumarol.
Élimination
L'acénocoumarol est éliminé du plasma avec une demi-vie de 8 à 11 heures. Après administration orale, la clairance plasmatique apparente est d'environ 3,65 L/h. La clairance plasmatique totale de l'énantiomère R (+) qui possède une activité anticoagulante significativement plus élevée, est plus faible. que celle de l'énantiomère S (-).
Seulement 0,12-0,18 % de la dose est excrétée sous forme inchangée dans les urines. L'excrétion cumulée des métabolites et du principe actif inchangé pendant une semaine équivaut à 60 % de la dose dans les urines et à 29 % de la dose dans les selles.
Populations particulières
Patients âgés
Dans une étude, des concentrations plasmatiques plus élevées d'acénocoumarol (qui produit certains taux de prothrombine) ont été observées chez des patients de plus de 70 ans après la même dose quotidienne que chez des patients plus jeunes.
Insuffisance rénale
Aucune information n'est disponible sur la pharmacocinétique clinique de l'acénocoumarol dans l'insuffisance rénale. Compte tenu de l'élimination urinaire de l'acénocoumarol, la possibilité d'une accumulation de métabolites en cas d'insuffisance rénale ne peut être exclue. Par conséquent, l'utilisation de l'acénocoumarol est contre-indiquée chez les patients présentant une insuffisance rénale sévère et des précautions doivent être prises chez les patients présentant une insuffisance rénale légère à modérée (voir rubriques 4.2, 4.3 et 4.4).
Insuffisance hépatique
Aucune information n'est disponible sur la pharmacocinétique clinique de l'acénocoumarol dans l'insuffisance hépatique. Sur la base du métabolisme de l'acénocoumarol et des activités enzymatiques éventuellement réduites, la clairance des CYP2C9, CYP1A2 et CYP3A4 est susceptible d'être réduite. Par conséquent, l'utilisation de l'acénocoumarol est contre-indiquée chez les patients. en cas d'insuffisance hépatique sévère et des précautions doivent être prises chez les patients présentant une insuffisance hépatique légère à modérée (voir rubriques 4.2, 4.3 et 4.4).
Ethnicité
Les systèmes enzymatiques du CYP2C9 sont exprimés de manière polymorphe et leur fréquence diffère d'une population à l'autre. Chez les Caucasiens, les fréquences d'occurrence du CYP2C9 * 2 et du CYP2C9 * 3 sont respectivement de 12 et 8 %. Chez les patients africains, les CYP2C9 * 2 et CYP2C9 * 3 apparaissent à des fréquences alléliques de 1 à 4 % et 0,5 à 2,3 % inférieures, respectivement, à celles des Caucasiens La population japonaise a des fréquences alléliques inférieures de 0,1 % et 1 à 6 % pour le CYP2C9 * 2 et le CYP2C9 * 3, respectivement.
La dose d'entretien d'acénocoumarol diffère selon le génotype.
Des informations détaillées sur la dose d'entretien moyenne et médiane basées sur le génotype du CYP2C9 sont fournies dans le tableau ci-dessous :
Tableau 3 - Dose d'entretien d'acénocoumarol selon le génotype du CYP2C9
05.3 Données de sécurité précliniques
Toxicité
Après une dose unique par voie orale et/ou intraveineuse, l'acénocoumarol a montré une légère toxicité chez la souris, le rat et le lapin.Chez le chien, il a montré une toxicité orale aiguë élevée.
Dans les études à doses répétées, le foie était le principal organe cible de la toxicité des dérivés de la coumarine, y compris l'acénocoumarol.Une administration pharmacologiquement excessive de ces substances peut provoquer des saignements.
Toxicité pour la reproduction et tératogénicité
Aucune étude animale n'a été menée avec l'acénocoumarol. Cependant, une interférence placentaire et transplacentaire avec des facteurs de coagulation vitamine K dépendants peut entraîner des malformations embryonnaires ou fœtales et des hémorragies chez les nouveau-nés, animaux et humains (voir rubrique 4.6).
Mutagenèse
Dans des tests in vitro effectués sur des lignées cellulaires bactériennes ou de mammifères, y compris un test de réparation de l'ADN dans des hépatocytes de rat, l'acénocoumarol et ses métabolites n'ont induit aucun effet mutagène. Une étude in vitro sur des lymphocytes humains a montré une légère activité mutagène. Cependant, dans cette expérience , les concentrations efficaces d'acénocoumarol 188 et ≥ 250 mcg/ml (en présence et sans activation métabolique, respectivement) étaient 500 à 1000 fois supérieures à celles déterminées dans le plasma humain après administration du médicament.
Carcinogenèse
Aucune étude de cancérogénicité chez l'animal n'a été réalisée avec l'acénocoumarol. La coumarine a induit une incidence accrue de tumeurs pulmonaires et de tumeurs hépatiques bénignes chez la souris et de tumeurs hépatiques et de tumeurs rénales bénignes chez le rat. Les tumeurs hépatiques chez le rat et les tumeurs chez la souris sont connues pour être associées à des voies métaboliques spécifiques à ces espèces.
Il est connu que l'hépatotoxicité de la coumarine et de ses dérivés chez le rat est associée à une induction enzymatique et que la biotransformation de la coumarine et/ou de ses métabolites est caractéristique de cette espèce de rongeur. Les tumeurs rénales observées chez les souris mâles sont considérées comme des effets spécifiques à l'espèce.
06.0 INFORMATIONS PHARMACEUTIQUES
06.1 Excipients
Comprimés de Sintrom 1 mg: silice colloïdale anhydre ; hypromellose; lactose monohydraté; stéarate de magnésium; fécule de maïs; talc.
Sintrom 4 mg comprimés: silice colloïdale anhydre ; lactose monohydraté; stéarate de magnésium; fécule de maïs; amidon de maïs prégélatinisé.
06.2 Incompatibilité
Pas d'instructions particulières.
06.3 Durée de validité
Comprimés de Sintrom 1 mg: 3 années
Sintrom 4 mg comprimés: 5 années
06.4 Précautions particulières de conservation
Ce médicament ne nécessite aucune condition particulière de conservation.
06.5 Nature du conditionnement primaire et contenu de l'emballage
Blister PVC opaque non toxique (ou PVC/PE/PVDC)
Comprimés de Sintrom 1 mg: 20 et 100 comprimés
Sintrom 4 mg comprimés: 20 comprimés quadrisécables
06.6 Instructions pour l'utilisation et la manipulation
Pas d'instructions particulières
07.0 TITULAIRE DE L'AUTORISATION DE MISE SUR LE MARCHE
Novartis Farma S.p.A.
Largo Umberto Boccioni, 1 - 21040 Origgio (VA)
08.0 NUMÉRO D'AUTORISATION DE MISE SUR LE MARCHÉ
Comprimés de Sintrom 1 mg - 20 comprimés - A.I.C. : 011782024
Comprimés de Sintrom 1 mg - 100 comprimés - A.I.C. : 011782036
Sintrom 4 mg comprimés - 20 comprimés - A.I.C. : 011782012
09.0 DATE DE PREMIÈRE AUTORISATION OU DE RENOUVELLEMENT DE L'AUTORISATION
Comprimés de Sintrom 1 mg Autorisation : 31.10.1994 Renouvellement : 01.06.2010
Sintrom 4 mg comprimés Autorisation : 6.11.1956 Renouvellement : 01.06.2010
10.0 DATE DE RÉVISION DU TEXTE
Décision AIFA de février 2015