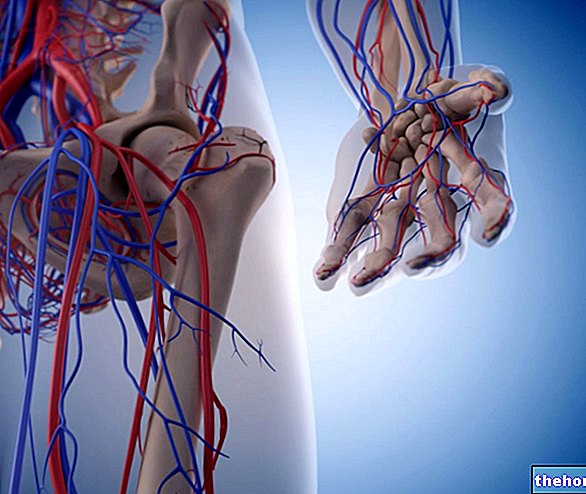
Après avoir été administré, le médicament est absorbé, entre dans la circulation, est distribué de la manière vue ci-dessus et atteint finalement le site cible où il exerce sa fonction pharmacologique.
Une fois que le médicament a fait toutes ses actions, il est éliminé de notre corps. Pour être éliminé, le médicament doit avoir les caractéristiques inverses par rapport aux caractéristiques utiles pour l'absorption ; pratiquement la substance administrée doit devenir hydrophile et inactive. son retour dans la circulation augmente sa permanence dans l'organisme et, bien entendu, tous les effets pharmacologiques fournis par le médicament sont également accrus.
Le but de notre métabolisme est de transformer le composé d'origine en un métabolite inactif, plus polaire que la molécule d'origine et de poids moléculaire inférieur. Cette intervention d'inactivation de la substance pharmacologiquement active se produit grâce à la présence d'enzymes particulières qui se trouvent principalement dans le foie. Certains médicaments après la phase de métabolisme peuvent donner naissance à différents métabolites, rencontrant ainsi des destins différents. Il n'est pas toujours certain qu'une substance inactive provienne d'une substance active, mais d'autres composés actifs, inactifs ou toxiques peuvent être générés. Une chose importante à mentionner est que les métabolites actifs peuvent également être générés à partir d'un composé inactif. Le composé inactif considéré est un promédicament qui, dans sa forme d'origine, est inactif et ne libère des métabolites actifs qu'après métabolisation.

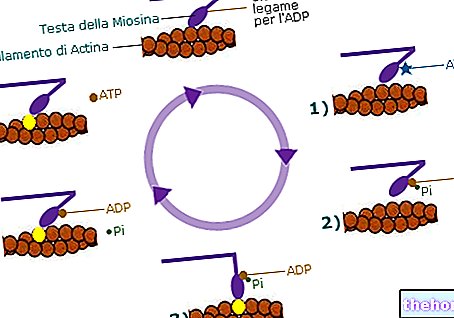
Réactions de phase I et de phase II dans la biotransformation des médicaments. Les réactions de phase II peuvent également précéder les réactions de phase I.
Grâce à l'étude du métabolisme, il est possible de déterminer la posologie du médicament en fonction de la maladie, la formation éventuelle d'autres composés, de prédire d'éventuelles interférences et enfin de prédire les changements de réponse suite à des traitements prolongés (induction et répression enzymatique). se produit principalement dans le foie, mais aussi dans les poumons, les reins, l'intestin, le placenta et la peau, grâce à des enzymes particulières. Ces derniers sont présents un peu partout, ont un nombre élevé et une faible spécificité de substrats (ils reconnaissent divers types de substrat et ont une faible efficacité catalytique). Ce déficit est compensé par les autres caractéristiques (présence élevée et nombre élevé).
Le métabolisme peut être de deux types : systémique ou présystémique. On parle de métabolisme présystémique lorsqu'une prodrogue doit être hydrolysée ou réduite pour obtenir un composé actif avant d'entrer dans la circulation ; ce n'est qu'à ce stade que le produit peut être absorbé et atteindre le site d'action. Dans le cas du métabolisme systémique, toutes les autres enzymes sont localisées dans des tissus qui ne sont atteints par les substances pharmacologiques qu'après avoir exercé leur action pharmacologique.
BIOTRANSFORMATION :
il se produit principalement dans le foie, mais aussi dans l'intestin, les reins et les poumons ;
la fonction principale du métabolisme est de transformer les substances lipophiles (qui sont difficilement éliminées par l'organisme) en composés hydrophiles qui peuvent être facilement éliminés.
ENZYMES, ENZYMES MITOCHONDRIALES ET MICROSOMIQUES
Jusqu'à présent, nous avons parlé d'enzymes, mais quelles sont-elles? Où sont? Quelle fonction ont-ils ? Ces enzymes sont des protéines et peuvent être trouvées partout dans le sang, le système digestif, le foie et le système nerveux central.
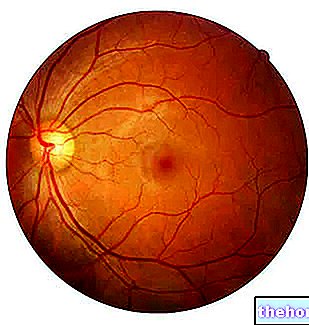
Dans la circulation sanguine, nous pouvons trouver des enzymes estérases qui catalysent l'hydrolyse des esters, des protéases et des lipases se trouvent dans le système digestif, le système enzymatique des monooxygénases peut être trouvé dans le foie et enfin dans le SNC les enzymes nécessaires à la dégradation des neurotransmetteurs. Toutes ces enzymes sont localisées dans les différents tissus cités plus haut, mais au niveau de chaque organe elles se trouvent généralement à l'intérieur de la cellule. Au niveau cellulaire elles peuvent être localisées dans l'espace extracellulaire ou intracellulaire. Si ces enzymes se trouvent dans l'espace extracellulaire l'espace leur activité est celle de dégrader des substances qui peuvent endommager la cellule, en fait elles sont aussi appelées enzymes pour protéger la cellule. Si elles se trouvent dans l'espace intracellulaire, elles sont principalement localisées dans les mitochondries, dans le cytosol et au niveau niveau.
Les mycorsomes sont des vésicules lisses et rugueuses du réticulum endoplasmique obtenues artificiellement par centrifugation. Ce processus de centrifugation n'a lieu que lorsque vous souhaitez subdiviser les composants subcellulaires d'une cellule. Les enzymes mitochondriales sont qualitativement et quantitativement prévisibles (nombre établi par le code génétique de la cellule, donc un certain nombre et un certain type seront formés), tandis que les enzymes microsomales ont un nombre et une "activité" variables. En fait, les enzymes microsomales sont responsables de les activités hypotrophiques ou hypertrophiques (augmentation ou diminution du nombre d'enzymes) et l'activité peuvent être modifiées en fonction des conditions auxquelles la cellule doit faire face.
Exemples de médicaments qui augmentent le métabolisme d'autres médicaments
INDUCTEUR
Médicament dont le métabolisme est augmenté
Phénylbutazone (anti-inflammatoire)
Cortisol, digoxine
Phénytoïne (antiépileptique, névralgie du trijumeau)
Cortisol, digitoxine, théophylline
phénobarbital et autres barbituriques
Anticoagulants, barbituriques, chlorpromazine, cortisol, phénytoïne,
Rifampicine (antibiotique qui inhibe l'ARN polymérase)
Anticoagulants, digitoxine, glucocorticoïdes, contraceptifs oraux, propranolol
Exemples de médicaments qui diminuent le métabolisme d'autres médicaments
INHIBITEUR
Médicament dont le métabolisme est inhibé
Cimétidine (antihistaminique anti-H2)
Diazépam, warfarine
Dicumarol (anticoagulant)
Phénytoïne
Disulfirame (alcoolisme)
Éthanol, phénytoïne, warfarine
Phénylbutazone (AINS anti-inflammatoire)
Phénytoïne
Autres articles sur "Elimination d'un médicament : réactions de biotransformation"
- Tératogénèse, médicaments tératogènes
- Transformations d'un médicament : réactions de phase 1